Background: Quality of life remains severely compromised in patients suffering from Transfusion Dependent Thalassemia (TDT) despite optimal supportive care. HSCT with a MSD, the current curative option, achieving a 92.1% 2y-OS in children and 84.4% in adults (EBMT registry). Unfortunately, availability of MDs is limited, so that haploidentical HSCT is increasingly explored.
Methods: 13 TDT patients (median age: 11 years; range: 2-23) received either a CD3 +/CD19 + (n=4; all class II/III) or αß/CD19 + (n=10; 7 class II, II/III) T-haplo-HSCT and were compared with 8 TDT-patients (7 class II, II/III, III) receiving a BM graft from a MSD (median age: 11 years; range: 4-22). Indication for T-haplo HSCT patients was severe iron overload/ transfusion-associated complications. All patients received an identical conditioning regimen consisting of treosulfan, thiotepa, fludarabine (FTT) and ATG-Grafalon, with the only difference in the timing of ATG (upfront in T-haplo-HSCT, prior to d0 in MSD-HSCT). Immunosuppression (IST) was maintained for a minimum of 180 days consisting of calcineurin inhibitors (mainly tacrolimus) and MMF.
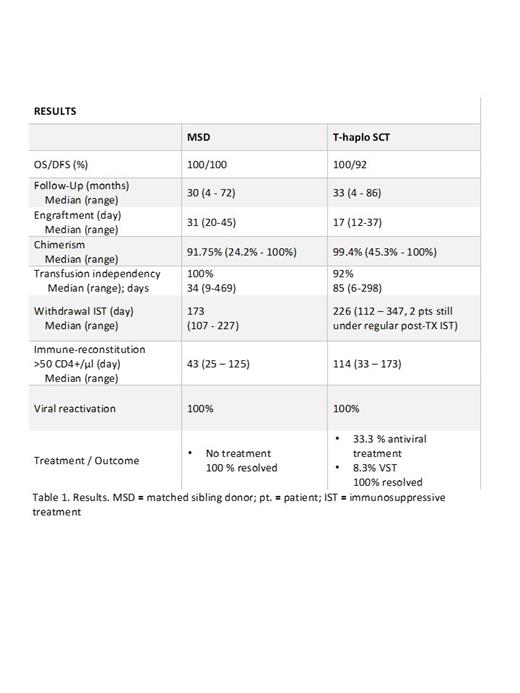
Results: The OS and DFS for MSD and T-haplo-HSCT was 100%/100% and 100%/92%, respectively (Table 1). The median follow-up was 30 months for MSD (range 4-72) and 38 months for T-haplo-HSCT (range 4-86). Neutrophil engraftment was achieved after a median of 31 days for MSD patients and 17 days for T-haplo-HSCT with a median of 5 x 10 8 TNC/kg (range: 3.28-7.88) and 15 x 10 6 CD3 +/CD19 + or αβ/CD19 + depleted CD34 + cells/kg (range: 9.2-24.2), respectively. One patient received two T-haplo HSCT, due to primary graft failure partly due to a major AB0 incompatibility. A mixed chimerism was observed in 3/7 MSD-HSCT (median 92%; range 27.5-100%) and in T-haplo-HSCT in 2/13 patients (median 99%; range: 45.3 -100%). Transfusion independence was achieved in all MSD and in all but one T-haplo patient. In MSD and in T-haplo-HSCT, IST was terminated after a median of 173 days and 226 days (range: 112-347), respectively. MSD patients reached CD4 counts >50/µl on day +43 (median; range: 25-125) and T-haplo-HSCT patients on day +114 (median; range: 33-173). The treosulfan-based conditioning regimen was well tolerated with no VOD/SOS observed in this high-risk population. No case of acute or chronic Graft-versus-Host disease (GvHD) was observed in the MSD population. In T-haplo-HSCT, 3 patients experienced grade I acute GvHD (skin) which resolved with prednisolone and in 2 cases with additional extracorporeal photopheresis. Only the oldest patient experienced mild chronic skin GvHD, which resolved by day +580. No severe infectious complications occurred despite a prolonged chimerism-triggered weaning of the IST.
Conclusions: Independent of donor availability, graft rejection and iron-overload related organ damage (VOD/SOS) are major pitfalls in transplanting advanced stage TDT patients. Treosulfan demonstrated to be an excellent alternative to busulfan in this setting reflected in the safety and efficacy data of this pilot series. Overall, outcomes of T-haplo-HSCT in TDT are very encouraging with a competitive OS, so that a transplant indication in pediatric and AYA TDT patients lacking a MD is feasible.
Disclosures
Wolff:Mallickrodt: Honoraria; Novartis: Honoraria, Research Funding; Incyte: Honoraria; Sanofi: Honoraria; Behring: Honoraria; Takeda: Honoraria; Gilead: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal